The results of Kristen's PET scan showed two lymph nodes lighting up, one in the gastro-hepatic area of her abdomen and the other in the lining of her esophagus.
While it could just be inflammation, Dr. Ali wants her to see a gastroenterologist but...
The results of Kristen's PET scan showed two lymph nodes lighting up, one in the gastro-hepatic area of her abdomen and the other in the lining of her esophagus.
While it could just be inflammation, Dr. Ali wants her to see a gastroenterologist but the earliest appointment is almost two months away.
Puzzling through the scenarios (as if she has a choice), Kristen hopes for a second, new kind of cancer rather than stage four, metastasized breast cancer.
Support the Breast Cancer Stories podcast
Subscribe to our newsletter
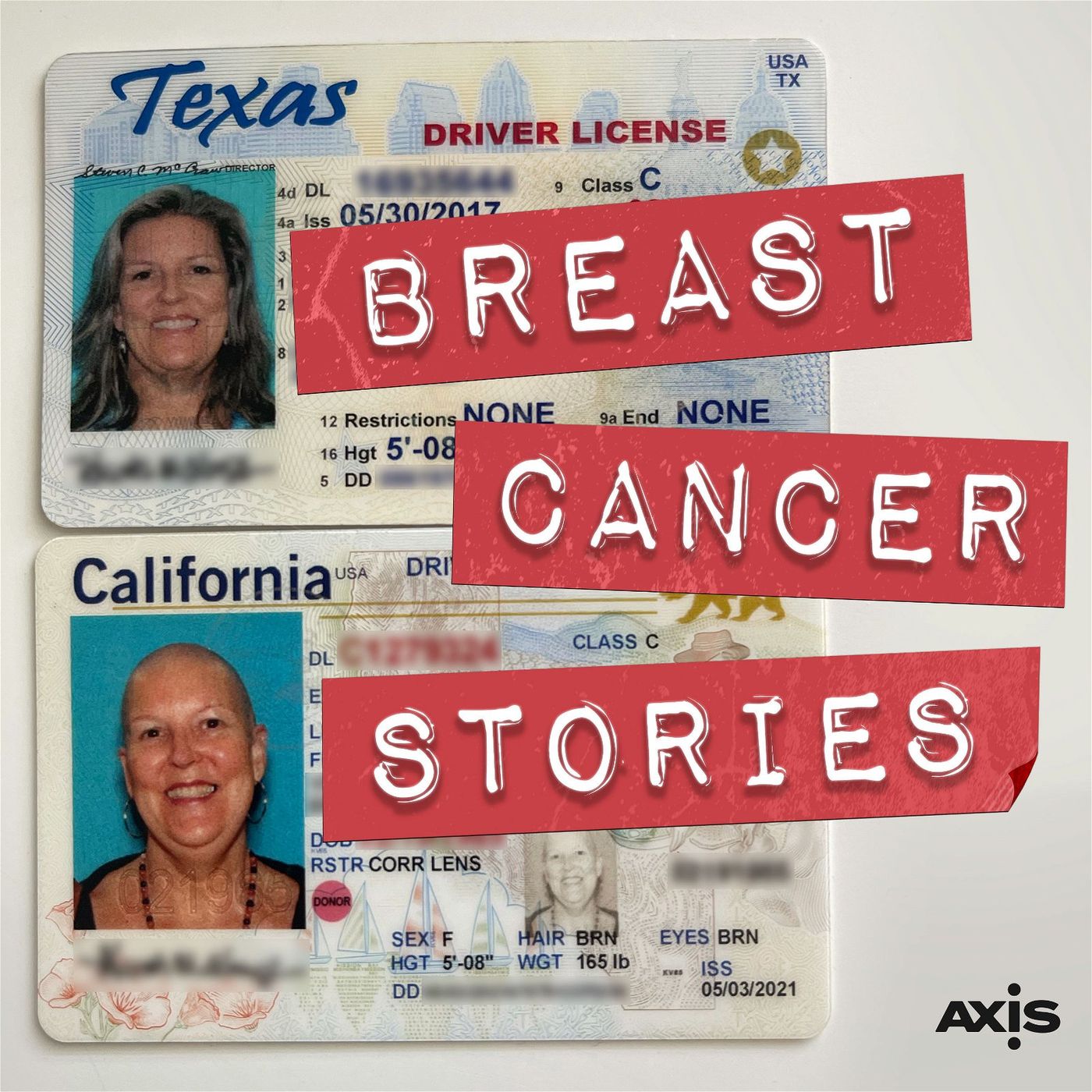
This podcast is about what happens when you have breast cancer, told in real time.
Host and Executive Producer: Eva Sheie
Co-Host: Kristen Vengler
Editor and Audio Engineer: Daniel Croeser
Theme Music: Them Highs and Lows, Bird of Figment
Production Assistant: Mary Ellen Clarkson
Cover Art Designer: Shawn Hiatt
Assistant Producer: Hannah Burkhart
Breast Cancer Stories is a production of The Axis.
PROUDLY MADE IN AUSTIN, TEXAS

The results of Kristen's PET scan showed two lymph nodes lighting up, one in the gastro-hepatic area of her abdomen and the other in the lining of her esophagus.
While it could just be inflammation, Dr. Ali wants her to see a gastroenterologist but...
The results of Kristen's PET scan showed two lymph nodes lighting up, one in the gastro-hepatic area of her abdomen and the other in the lining of her esophagus.
While it could just be inflammation, Dr. Ali wants her to see a gastroenterologist but the earliest appointment is almost two months away.
Puzzling through the scenarios (as if she has a choice), Kristen hopes for a second, new kind of cancer rather than stage four, metastasized breast cancer.
Support the Breast Cancer Stories podcast
Subscribe to our newsletter
This podcast is about what happens when you have breast cancer, told in real time.
Host and Executive Producer: Eva Sheie
Co-Host: Kristen Vengler
Editor and Audio Engineer: Daniel Croeser
Theme Music: Them Highs and Lows, Bird of Figment
Production Assistant: Mary Ellen Clarkson
Cover Art Designer: Shawn Hiatt
Assistant Producer: Hannah Burkhart
Breast Cancer Stories is a production of The Axis.
PROUDLY MADE IN AUSTIN, TEXAS
Updates to keyboard shortcuts … On Thursday, August 1, 2024, Drive keyboard shortcuts will be updated to give you first-letters navigation.Learn more
bcs048
Eva (00:07):
This is a story about what happens when you have breast cancer told in real time. And she's back.
Kristen (00:16):
Yay.
Eva (00:19):
Why were we coming back? You must be okay.
Kristen (00:23):
We don't know that yet. We're coming back to talk about the results of the PET scan.
Eva (00:29):
When was that? About 10 days ago?
Kristen (00:32):
It was two weeks ago yesterday. So had the PET scan on June 5th, and I don't even really know how to talk about this. Once again, I was with Sam. We were at the Safari park. And so I went in really early in the morning, it was like 6:00 AM and they injected some stuff. And there was a metal box that had a vial that there was a lock on the metal box, the metal box opens, a vial comes out, and then they inject it in. I was like, oh, that's cool. I think it's the radiation or the whatever it was that was going in me for the PET scan.
Eva (01:14):
Whoa.
Kristen (01:16):
It was very weird. Anyway, I've never had one before. I sat there for 45 minutes for the dye to get in, and then I went in and it's kind of like an MRI, except it doesn't really close. You just go through a hoop and it took about 15 minutes.
Eva (01:40):
Cuz it moves really slowly?
Kristen (01:42):
You're just kind of going back and forth. I think it's just that that's how long it took to take the images. And I wish Natasha was here to explain it to me, but I think whatever they put in, it's supposed to light up places in your body that have activity, which doesn't always mean it's cancer. I've learned that inflammation can do that. So anyhow, I have the PET scan really early in the morning and Sam and I go to the Safari Park and I really wasn't expecting anything because they said, oh, this is a Wednesday. They said, oh, we'll have your results to your doctor by the end of the week or early next week. And I was like, oh, good, you know it'll be a reprieve. So Sam and I are sitting there having a pretzel cruising around and I see, oh, new test results in the portal. And I was like, oh, of course, right? Because that's what I do. And I opened it but didn't really read it. I just kind of scanned it and then was like, just forget it. They'll call you. And so then I see that I missed a call from Dr. Ali's nurse and she said, I see that you've looked at the PET scan. And then she leaves me this message about what Dr. Ali wants to do and all the things.
(02:57):
So this is a Wednesday. I had already set up an appointment to see Dr. Ali the following Monday.
Eva (03:03):
It's still the same day that you had it.
Kristen (03:05):
Right?
Eva (03:06):
Which is you weren't expecting to hear?
Kristen (03:08):
No.
Eva (03:10):
Okay.
Kristen (03:10):
No.
Eva (03:10):
So are you worried already because just because it's the same day and they're calling you?
Kristen (03:17):
Mm-hmm. Well, and I saw there was a missed call from a Scripps number. I didn't know who it was, but you know how on your phone, it's like visual voicemail, you can kind of see. So then I went in and looked because I wasn't in a place where I could really go and have a conversation.
Eva (03:39):
Well, you sent it to me. It was not easy to read. It's crazy medical language and abbreviations and words that we don't know. And so you definitely need somebody to explain everything to you.
Kristen (03:52):
Yeah, hence Google.
Eva (03:53):
Yeah. Okay, so reliable.
Kristen (03:57):
Well, what it does do is it explains a meaning. I don't chain all the things together. I just do 'em independently. Anyway, so what was surmised from that is that lymph node, I'm going to sound like I really know what I'm talking about. Ready? The gastro hepatic ligament lymph node, which is the ligament that connects the liver and the stomach, the one we didn't know we had. That lymph node lit up as did the lining of my esophagus. And so Dr. Ali said that this is not a common place for breast cancer to recur in that gastro hepatic area. And so she referred me to a gastroenterologist to get a consult, and actually it was basically like, Hey, get an endoscopy and a biopsy on this stat. And so I'm referred over there, and then there were two more lymph nodes that lit up. They were not enlarged.
(05:05):
They are what are called the level two cervical, which is kind of like by your jugular veins back in here behind your chin. And I would imagine those are the ones that when you have a cold, people say you have swollen glands, that those are the ones that swell. So the two lymph nodes on that side both lit up. So Dr. Ali, when I saw her, she said, well, I don't really think we need to do a biopsy right now. Let's do another PET scan in three months and keep an eye on those. Prudent, right? The soonest they could get me in to see a gastroenterologist is July 23rd. I called on June 6th. I called every gastro in the Scripps network and each location, as I do.
Eva (06:00):
You're calling them every morning just like you were with
Kristen (06:03):
I am, I am actually every morning and every afternoon. And there are only two advanced gastros or specialists like advanced guys that can do this kind of thing in the network. And so that's why it's taking so long to get in. So when I call, what I say is, I'm sorry to bother you guys. I just have to tell you I'm a little nervous. My oncologist said I need to get in as soon as I can to see you guys. I've had breast cancer before, just a little nervous. And what I'm kind of up against is, wow, it's taking me almost two months to get in to see you guys. How long is it going to take after the consult to get the endoscopy? Is it going to be another two months because I was supposed to see you urgently. And so finally today, about an hour ago, I did call again and she said, oh, we'll put you on, you're still on the constellation list. And I said, thank you so much, and I really appreciate everything you guys are doing. Is there any way you can put a note into the nurse so they can call me and see if I can get an earlier? And I said, I'm really sorry, I'm just really, really nervous about this. So I'm sure it's fine that I'm waiting. I am sure they'll get me in quickly, but I don't know. It is just weird that when something,
Eva (07:22):
Yeah, but you don't want the reason that something got worse or you don't want to look back and say, if I'd gotten in sooner, maybe they could have caught whatever.
Kristen (07:33):
Right.
Eva (07:35):
And these are not like, wait till next week. These are wait two months. It's too long.
Kristen (07:40):
Right. I agree. I agree. Well, and in the meantime, so where are we? We are waiting for more information to know what's going on with this. Dr. Shimizu is the radiation oncologist that took over my case when Dr. Coco has moved locations. And so I went ahead and a while back, scheduled an appointment with him, and just so happens all this stuff is in the file now since I scheduled that appointment with him. And I don't know, I mean, it's kind of like I resigned myself to, oh, you know what? That lymph node is just agitated because of all the gastro stuff that's going on right there. I talk myself out of all the what ifs. And I go see Dr. Shimizu. It did take a little bit of courage to walk into the radiation center again because it hits where his office is. It's like going for my infusion in the chemo center again.
(08:40):
It's just, it's a little trigger. But anyhow, so he was talking and he said, I reviewed everything. And he says, and I know, I know he's a scientist. I know, and he's looking at data, and he just looked at my file, and he's looking at it as, what are our next steps? He said, so the spot in your abdomen, he said, if it's related to the breast, we'll probably just do some radiation. If it's not related to the breast, then probably some chemo and radiation is what's probably going to happen. And then he does an exam and he checks everything. And this was new information to me. He said, the tumor has to be really big in the esophagus for it to be caught on a PET scan. When they go in to do an endoscopy, they're going to do an ultrasound that looks at that lining because there can be a small tumor in that lining that's thickened in the esophagus.
(09:46):
And I was like, hmm. I mean, I was like, okay. And so then we're finishing everything up and I said, I'll see you in a year because this isn't going to be anything. And he said, I hope so. And he said, but do send me a note in the portal as soon as you have the biopsy. And that way that will trigger me to go in there and take a look and see what we need to do. And so I know that he was just giving me the information, but there's also something inside of me that's like, what is he seeing and what has he seen through his experience that I don't know. And so of course, I went back and read his notes. I always go back and you can go in and read the notes that they put. And so it says in here, Kristen Vengler is seen in a brief recheck for new hypermetabolic gastro hepatic lymph node as the only site of active disease on the PET CT scan. And then he goes through, and then he gives my whole history. And so I want to say this the correct way. So it says, intensely avid single gastro hepatic lymph node. Given the small hiatal hernia with moderately avid esophageal gastric wall thickening that may represent esophagitis, although underlying neoplasm, meaning an underlying tumor is difficult to exclude.
(11:18):
And it says non-specific, non enlarged bilateral cervical level two lymph nodes, possibly reactive.
Eva (11:25):
Does it make anybody else crazy that cervical means both neck and cervix?
Kristen (11:29):
Yes, 200%. When I saw a cervical lymph node in there, I was like,
Eva (11:35):
You thought it was cervical cancer, right?
Kristen (11:37):
Yes. My mom had ovarian. I keep up on all of those parts.
Eva (11:44):
Yeah.
Kristen (11:44):
So the bottom line is where are we? We're in a pretty good spot in the sense that the PET scan did give really good information about no bone. There's nothing in my bones, nothing in my organs, nothing in my other tissues. It's these lymph nodes and the esophagus that are issues, which is fantastic news considering how advanced my cancer was. So we're waiting to see the gastro in a month unless I can get in earlier, and then we're waiting on another PET scan in September. And what I have really realized through this is that as much as we want our healthcare and cancer treatments to be linear, meaning that, oh, you had an ACL reconstruction, do these things and you're going to be good as new. Right. That's never true. My ACL still isn't, right.
Eva (12:44):
Oh, I missed that scooter. I just was seeing you rolling around on that thing. Okay. And in the history of stupid injuries, that was the stupidest.
Kristen (12:58):
Oh my.
Eva (12:59):
That was a different scooter injury. Am I thinking of a different thing? What happened at school?
Kristen (13:04):
No, I slipped in my classroom once.
Eva (13:07):
But why did you slip? There was some really idiotic reason that you slipped.
Kristen (13:10):
I was working late.
Eva (13:12):
Did they mop the floor or something?
Kristen (13:13):
And they mopped the floors and didn't put anything up. I'd gone to the bathroom and came back. I didn't know.
Eva (13:18):
Oh, I hate that one.
Kristen (13:20):
I know. It was ridiculous. Ridiculous. But it's kind of like you're used to take this antibiotic, take this when you're not feeling well, this will get you back to a hundred percent. And I just really realized that cancer care isn't linear. It's always kind of in process. And so I've really, really had to work on what I call my time travel and my what ifs. I have to really stay in the moment and realize that it's going to be what it's going to be. My stepmom was in town and I saw her last night. I hadn't seen her since I'd been diagnosed before. And we were talking about things and showing her my boobs and all the things you do. And I told her that there were some things pending that we were looking at. And I found myself, again, taking care of others and how they were feeling because the way she was so mortified, I was like, oh, I shouldn't have said anything.
(14:23):
And then my sister came and she'd hidden and gone, and she was asking, Hey, what's going on? And so I'm explaining it, and my brother-in-law's there and everything, and I said, but I've been through the chemo, I've been through the radiation. I've been through the surgeries. I found myself saying to my sister and my brother-in-Law is like, you know what? I've been through everything so far. If this is something, then I've been through whatever it is we need to do. And they're like, well, but if it's a different kind of cancer that's a second cancer. I said I would prefer, I can't believe I'm saying this. In what universe would I ever think I'm supposed to say this? If it is something in my esophagus or in my gastric area that's a new cancer, hopefully. I think it's a worse outcome if the breast cancer has traveled there, because that means it's stage four and it's metastasized. So I think it's really weird that I would prefer to have a second type of cancer. But what I think is funny is that I don't know if you remember, Natasha and I were talking about esophageal cancer because her esophagus was so messed up. She's like, I think I have esophageal cancer. And I'm like, no, you don't have esophageal cancer. And here I am saying that's what this could be.
Eva (15:47):
Yeah, you got to stop saying stuff, cuz you're just going to end up with it.
Kristen (15:51):
No, we're not going to manifest any of that. Anyway, so it's very interesting because I feel like we're in that place back at the end of 2020 when I was waiting for all the information and seeing all the doctors and figuring out what the treatment looked like. And it's a very different perspective because the first, I guess, response was kind of a trauma response of like, oh my gosh, I don't want to go through this again. And I'm realizing as I'm sitting here talking about this, I just did what I said I wasn't going to do. I just time traveled on all of it. But when I was having this conversation with people, I found myself watching their expressions. I found myself trying to take care of them and make them feel better about what my medical situation was. And I'm like, why, why? And I think it's just because there's a certain bravery and a certain knowing that you do when you've been through this stuff. And I'm talking to people who've never had cancer and who've seen me go through it, but it was just really interesting because I was having a conversation with them. I'd had the thought process of, I thought it was a weird thing for me to say, I hope it's a different type of, if it is something, it's a safer medical bet to have something new than to have a stage four, something.
Eva (17:33):
Interesting perspective. Kristen.
Kristen (17:36):
I don't know. I always ask you this. What does it sound like to you? I just, I'm in my head.
Eva (17:42):
Well we all have sort of an idea of how we should react. And so I think maybe what you're seeing is we think we're supposed to be scared and we think we're supposed to be worried, and to make it seem like we're, maybe it's genuine. But even going through it with you for the second time, my reaction is different too. And what did I say to you when you told me what happened? I said, well, you made it through breast cancer, so you're clearly invincible and they can just see you whenever they want.
Kristen (18:13):
Right. That's exactly what you said.
Eva (18:16):
I mean, I wasn't even, like I said, oh, hell no.
Kristen (18:20):
Yeah, yeah.
Eva (18:21):
It's different.
Kristen (18:24):
Isn't it weird?
Eva (18:25):
Yeah, it is weird. Another thing I've noticed is that people who had stage one or two, they're not like you.
Kristen (18:33):
In what way?
Eva (18:35):
To me, it seems like they don't really worry that much, and it wasn't really that big of a deal.
Kristen (18:41):
There aren't as many things that come up. Is that what you're saying? And I think that my doctors, based on what it was, that it was stage three B three C, I think it changed in there somewhere and that it was in the lymph nodes, I think that there's more caution. So I'm hoping that I get to see someone sooner and get something set up, but my guess is that it's probably, it's a month away from the consult. So I would hope that they would be able to get me in within a couple of weeks. So that's probably August.
Eva (19:22):
And if you don't, at least you know that you tried everything you could try to get in sooner.
Kristen (19:30):
Yeah. We'll see what happens. I feel hopeful. Yeah. I'm just trying to work it out so that I'm not thinking constantly about it. And I'm, I'm not going to sit and think about what Dr. Shimizu said, only area of active disease. What? Because I'm getting ready to be really excited that what is today, Thursday?
Eva (19:54):
Clearly he doesn't know you because you're also mentally ill.
Kristen (19:59):
<laugh> Have you met me? On Saturday is three years cancer free.
Eva (20:06):
Awesome.
Kristen (20:07):
Yeah, it was three years since my mastectomy. So I'm still going to celebrate that because it's true. And every day that goes by is better. And actually, was it two years, two years ago tomorrow, Dr. Pacella finished my reconstruction.
Eva (20:24):
A lot of anniversaries in June. So let's talk after you see the gastro in less than 33 days, hopefully, if there's anything interesting to say. I mean, I guess even if there's nothing that would be great. We can talk about.
Kristen (20:41):
Yeah.
Eva (20:41):
I do want you, I have been thinking, and it's up to you of course, as always, but I do think there's going to come a time, and it might be soon, it might not, that we will want to tell your story of what happened before you had cancer.
Kristen (20:58):
Oh.
Eva (20:58):
And it has enough time gone by for us to revisit that. I mean, that's on you to decide.
Kristen (21:06):
Yeah. It's interesting you say that because when I was talking to my stepmom, we're talking about just that I got cancer. And I didn't burden her with all the school stuff that had happened and all that. And I said, there's a book that's called How Not to Die by Dr. Gregor. Love Dr. Gregor. And now he has one called How Not to Age. But what he does say in there, and I really do believe it, is that we all have cancer cells that are dormant, and they could based on genetics, based on environment, based on our actions, based on our biology, they could come when we're 30, when we're 60, when we're 150. There are some things that we can do to not like smoking and all that. The four top causes of breast cancer, are stress, excessive alcohol, poor eating habits and smoking. And I didn't smoke, but in the two years before getting breast cancer, I was under extreme stress like most people never are in their life, I was drinking so much to numb all of that, that I went to rehab, I was eating a ridiculous amount. I would wake up in the morning and go, oh, you made that when you were drunk? Wow, that's a lot of food.
(22:37):
And I was telling her, I don't think she really put it together. But the other thing too is that my cancer is estrogen positive, and I was on synthetic estrogen because of menopause. And so there are all of these things, and maybe taking estrogen when I'm 50 and maybe drinking a lot when I'm 20, and maybe having stress when I'm 30. Maybe those things independently would not have triggered this, but in a very short period of time, all of those behaviors, all of those actions, all of those decisions just made it burst. And so I really feel like it's important for people to understand how to manage themselves through those situations. But I'm happy to talk about that whenever you'd like to. I don't have an NDA.
Eva (23:27):
Yeah, let's plan it. Okay, we'll see you soon.
Kristen (23:30):
Love you.
Eva (23:31):
Love you too. Thank you for listening to Breast Cancer Stories to continue telling this story and helping others. We need your help. All podcasts require resources, and we have a team of people who produce it. There's costs involved, and it takes time.
Kristen (23:48):
If you believe in what we're doing and have the means to support the show, you can make a one-time donation, or you can set up a recurring donation in any amount through the PayPal link on our website at breastcancerstoriespodcast.com/donate.
Eva (24:02):
To get the key takeaways from each episode, links to anything we've talked about and promo codes or giveaways from our partners, sign up for our email newsletter.
Kristen (24:12):
You'll get notes and thoughts from me related to each episode, and links to the most useful resources for all the breast cancer things. So if you have chemo brain, you'll be able to just go read your email, find anything we talked about on the podcast without having to remember it.
Eva (24:26):
The link to sign up is in your show notes and on the newsletter page at breastcancerstoriespodcast.com.
Kristen (24:32):
We promise not to annoy you with too many emails.
Eva (24:36):
Thanks for listening to Breast Cancer Stories. If you're facing a breast cancer diagnosis and you want to tell your story on the podcast, send an email to hello@theaxis.io. I'm Eva Sheie, your host and executive producer. Production support for the show comes from Mary Ellen Clarkson, and our engineer is Daniel Croeser. Breast Cancer Stories is a production of The Axis, THEAXIS.io.